Tylenol Autism Pregnancy
👶 Tylenol And Autism Pregnancy Claims & the Viral “Tylenol Challenge” Explained

“Tylenol autism pregnancy” is surging in search thanks to lawsuits, politics, and social feeds, while the “Tylenol challenge” (a TikTok overdose dare) keeps spiking attention cycles. Below we will busts myths, traces the rumor mill, and lays out what the science and official statements actually say.
Tylenol (acetaminophen) is one of the world’s most ubiquitous over-the-counter pain relievers, used by millions to treat headaches, fever, and aches scientificamerican.com. When taken as directed, it is generally safe and effective scientificamerican.com. Yet this common drug has recently made headlines for alarming reasons: a dangerous social media overdose “challenge” and controversial claims that prenatal Tylenol use might contribute to autism in children. In this in-depth explainer, we’ll examine how Tylenol works in the body, its safety profile, and the facts behind these high-profile issues – separating myth from reality with the latest evidence and expert commentary.
🧪 What Is Tylenol and How Does It Work?
Tylenol is the brand name for acetaminophen (known as paracetamol outside the U.S.), a medication first synthesized in the late 19th century scientificamerican.com. It’s classified as an analgesic (pain reliever) and antipyretic (fever reducer) goodrx.com. People worldwide reach for Tylenol to relieve mild to moderate pain – from headaches and muscle aches to menstrual cramps – and to reduce fevers from illnesses like colds or the flu goodrx.com. Unlike ibuprofen or aspirin, Tylenol is not an anti-inflammatory drug; it doesn’t reduce swelling or inflammation goodrx.com. This is because Tylenol works differently than those nonsteroidal anti-inflammatory drugs (NSAIDs).
How exactly does Tylenol relieve pain and fever? Surprisingly, scientists still aren’t completely sure. “Even though acetaminophen has been used for decades, we still don’t know exactly how it works,” one pharmacy article notes goodrx.com. However, there are several leading theories. The traditional explanation is that Tylenol interferes with the production of prostaglandins – chemical messengers that increase pain sensitivity and raise body temperature scientificamerican.comgoodrx.com. Tylenol appears to block certain cyclooxygenase (COX) enzymes in the brain and spinal cord, which in turn prevents formation of prostaglandins that would otherwise signal pain and fever goodrx.com. In essence, it “tricks” the brain’s pain and temperature regulation centers into dialing down discomfort goodrx.com. Because this action is largely limited to the central nervous system, Tylenol doesn’t have the anti-inflammatory and blood-thinning effects that NSAIDs do goodrx.com.
Another intriguing theory is that acetaminophen works through the body’s endocannabinoid system – the same system targeted by cannabis. Research from Indiana University in 2025 found that Tylenol inhibits an enzyme that produces 2-AG, a natural endocannabinoid molecule news.iu.edu. Counterintuitively, lowering 2-AG levels reduced pain responses in the study, suggesting Tylenol might ease pain by modulating our internal cannabinoid signals news.iu.edu. Other studies have shown that when Tylenol is metabolized, it produces a compound (AM404) that activates cannabinoid receptors and also affects serotonin pathways involved in pain perception scientificamerican.comgoodrx.com. In short, acetaminophen likely has multiple targets in the body. “Pain pathways are very complicated,” explains neuropharmacologist Alex Straiker, “so acetaminophen is likely to have multiple targets” scientificamerican.com – possibly prostaglandins, cannabinoids, serotonin, and more.
Exciting new discoveries are still emerging. In 2025, a team at Hebrew University revealed a previously unknown mechanism: Tylenol doesn’t only work in the brain; it also blocks pain at its source, in the nerves. They found that the metabolite AM404 actually shuts down specific sodium channels in pain-sensing nerve endings, stopping pain signals before they even reach the brain sciencedaily.comsciencedaily.com. This “revolutionizes our understanding of how this common medication works,” the researchers noted, and could spur development of better painkillers in the future sciencedaily.comsciencedaily.com.
The bottom line is that Tylenol’s mechanism is complex and still being studied. But despite the remaining scientific puzzles, its real-world effects are well-proven: it reliably reduces fever and alleviates many types of pain. That consistency and a relatively gentle side-effect profile (no stomach bleeding, for example, as seen with some NSAIDs) made Tylenol a medicine cabinet staple for generations. It’s this reputation for safety that makes the ongoing debates about a possible Tylenol autism pregnancy risk so striking.”
⚠️ Why Tylenol Is (Usually) Safe: Proper Use and Risks
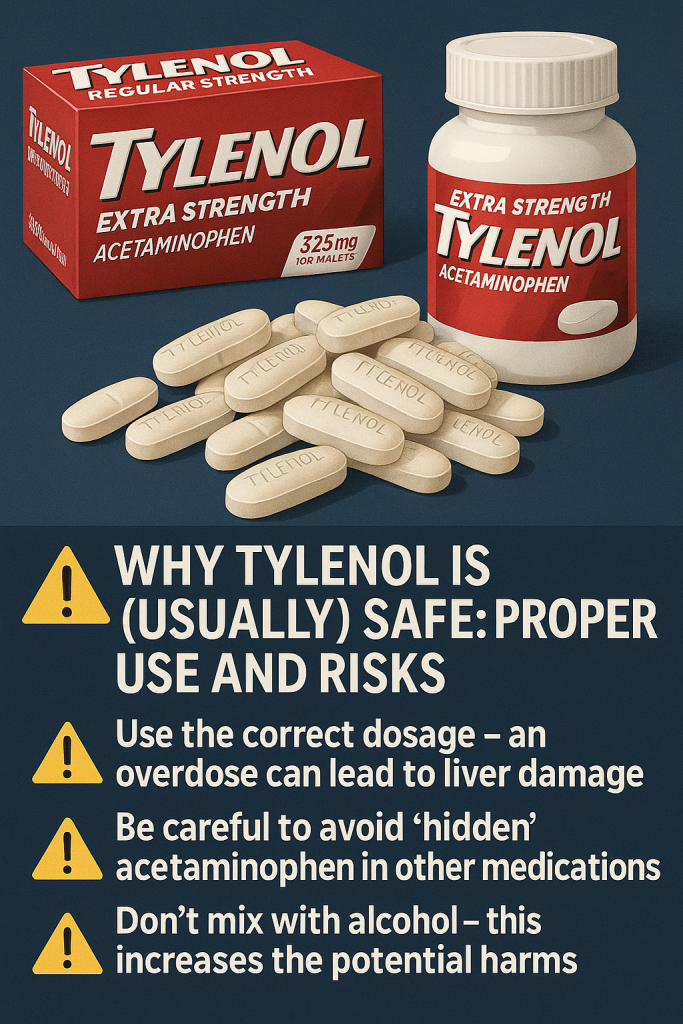
One reason Tylenol is so popular is its perceived safety. Unlike aspirin, it doesn’t irritate the stomach or cause bleeding, and it’s one of the few pain relievers considered safe for infants and pregnant women (more on pregnancy later). When used at the recommended dose, acetaminophen is very safe for most people scientificamerican.com. However, a critical caveat is often overlooked: Tylenol in high doses can be extremely dangerous, even deadly.
The therapeutic window for acetaminophen is narrower than many realize. The typical maximum adult dose is 4,000 mg per day (equivalent to eight extra-strength tablets), and some experts now recommend capping it at 3,000–3,250 mg to add a margin of safety goodrx.com. Exceeding these limits – whether by accident or on purpose – risks serious liver damage goodrx.comgoodrx.com. The liver breaks down acetaminophen, and too much of it overloads the liver’s normal metabolic pathways. This leads to the production of a toxic byproduct that can kill liver cells. In fact, taking too much Tylenol is the most common cause of acute liver failure in the United States mayoclinic.org. Each year, acetaminophen overdose sends thousands to the ER and causes an estimated 500 deaths in the U.S. alone news.iu.edu. It is also a leading cause of liver transplants worldwide news.iu.edu.
Tragically, many of these cases are unintentional. Acetaminophen is an ingredient in hundreds of over-the-counter products – from cold & flu remedies to prescription painkillers – so people sometimes double-dip without realizing it. For example, someone might take Tylenol for a headache and a multi-symptom cold medicine, not knowing both contain acetaminophen. Reading labels is essential: the FDA advises that the total 24-hour intake from all sources not exceed 4,000 mg goodrx.com. It’s also wise to avoid drinking alcohol when taking acetaminophen, since alcohol can worsen liver toxicity goodrx.com. As a rule of thumb, use the lowest effective dose for the shortest necessary time – this maximizes benefits and minimizes risk.
What actually happens if someone takes a massive overdose of Tylenol? Initially, there may be no obvious signs – which is part of the danger. The drug silently damages the liver over a day or two. “The first signs of poisoning may not appear until 24 to 48 hours after ingestion,” health authorities warn swissinfo.ch. By then, the person may develop nausea, abdominal pain, coordination problems, and alarming symptoms of liver failure like jaundice (yellowing of skin/eyes) swissinfo.ch. Without prompt medical treatment (such as the antidote N-acetylcysteine), acute liver failure can be fatal. This delayed onset is why overdoses can be especially insidious – people might not connect the dots or seek help until it’s too late. And unlike many drug overdoses, acetaminophen overdose usually isn’t immediately obvious to bystanders – there’s no dramatic unconscious collapse, just a slow and often hidden destruction of the liver.
In summary, Tylenol is very safe when used correctly, but extremely dangerous when misused. Over-the-counter does not mean “risk-free.” As Dr. Lee Dossett, a chief medical officer, put it: “It’s perfectly safe, except in excess…Taking multiple pills or a combination of things is very unsafe” wkyt.comwkyt.com. This point has been driven home in a disturbing new way by a recent social media phenomenon – the so-called “Tylenol Challenge.”
⚠️ The “Tylenol Challenge”: A Deadly Social Media Trend
In mid-2023, alarm began spreading about a viral TikTok dare dubbed the “Paracetamol Challenge” (paracetamol being the international name for acetaminophen). This social media challenge encourages teenagers to intentionally overdose on Tylenol/Paracetamol – essentially, to poison themselves – as a twisted competition. Participants reportedly challenge each other to ingest extremely high doses and then see who can stay hospitalized the longest as a result independent.co.ukemilyshope.charity. It’s a dangerous game of chicken with one’s health, and the consequences have already been tragic.
Authorities in the UK sounded the alarm in August 2023 after multiple teens in Southampton were hospitalized from overdosing on paracetamol as part of this trend independent.co.ukemilyshope.charity. “Young people, aged 15 to 17, decided to challenge each other to overdose. And the person who remained in hospital for the longest would be the winner,” explained Donna Jones, a British police commissioner, highlighting the recklessness of the act emilyshope.charity. Around the same time, Swiss doctors grew concerned as the challenge spread in Europe – several regions in Switzerland issued public warnings in early 2025 about the “fatal consequences” that can result swissinfo.chswissinfo.ch. Health officials even asked pharmacies to be vigilant about selling paracetamol to minors swissinfo.ch.
Unlike some internet stunts that are fake or exaggerated, this one has had real victims. A 13-year-old in Ohio died in 2023 after attempting a related “Benadryl Challenge” (overdosing on allergy medicine to induce hallucinations) emilyshope.charity. In his case, the boy took 12 to 14 Benadryl pills, had a seizure on camera, and never recovered emilyshope.charity. While that involved a different drug, it underscores the broader trend of teens misusing common medicines to chase viral fame – with deadly results. The paracetamol/Tylenol challenge poses a similar threat. Doctors warn that massive acetaminophen doses will destroy the liver and can easily be lethal swissinfo.chswissinfo.ch. Even those who survive may require liver transplants or face lifelong health issues.
Equally troubling is the mindset behind the challenge. The fact that adolescents consider an OTC painkiller “safe enough” to abuse in this way speaks to a misconception that needs busting: Just because a drug is sold without a prescription doesn’t mean it can’t kill you. As one charity monitoring youth substance trends put it, easy access to household medicines plus peer pressure and viral dares is a dangerous mix emilyshope.charity. The U.S. FDA has urged parents to talk to their kids about such risks, emphasizing that “overdoses can happen with OTC drugs just as easily as with prescription medications” emilyshope.charity.
In response to the TikTok challenge phenomenon, schools and police have been spreading warnings. TikTok, for its part, claims it has seen no evidence of the trend on its platform independent.co.uk – a common refrain from social media companies facing bad press. Regardless of its origins, the Tylenol challenge is a toxic and potentially deadly dare. It serves as a harsh reminder that misusing Tylenol – even just to “see what happens” or to impress friends – can lead to irreversible harm.
👶 Does Tylenol Cause Autism? Investigating the Tylenol Autism Pregnancy Controversy
Apart from social media crazes, Tylenol has been caught up in another storm – one that has unsettled many parents and even reached the halls of government. The question at hand: Does using acetaminophen during pregnancy increase the risk of autism or ADHD in children? It’s a claim that has circulated for years in scientific circles and recently exploded into public debate, fueled by lawsuits and political statements. Let’s unpack what we know – and don’t know – about this contentious topic.
📜 Tracing the Origins of the Claim
Researchers have studied acetaminophen’s effects on child development for nearly four decades washingtonpost.com. The idea of a Tylenol autism pregnancy connection began surfacing in the 2010s. Early investigations mostly found no clear link. However, in the 2010s some large observational studies reported a possible association between prenatal acetaminophen use and a higher incidence of neurodevelopmental disorders. Notably, two influential studies (in 2016 and 2019) found that children whose mothers took a lot of Tylenol during pregnancy had higher rates of autism and ADHD diagnoses washingtonpost.com. The increase in risk was modest, but enough to raise eyebrows. Then in 2021, 13 scientists authored a consensus statement urging caution – they recommended that pregnant women use Tylenol “at the lowest effective dose for the shortest possible time” washingtonpost.com. This statement, published in a leading journal, didn’t claim acetaminophen is proven dangerous, but it did reflect growing concern in the research community.
It’s important to understand what these studies actually show. They are observational studies, meaning researchers followed populations over time and looked for correlations. For example, one study might track thousands of mother-child pairs and find that those who reported frequent acetaminophen use had, say, a 20% higher rate of autism diagnoses in their kids. Correlation, however, does not equal causation. Many experts note that it’s extremely challenging to prove a direct cause-and-effect link between an exposure (like a medication) and a complex outcome like autism washingtonpost.com. There are many confounding variables that could be in play. Perhaps women who needed a lot of pain relief during pregnancy had underlying infections or inflammation that affected the baby’s development, not the Tylenol itself. In fact, one of the very factors Tylenol is used for – fever – is known to pose risks to a developing fetus (high maternal fever in early pregnancy can lead to birth defects). So some hypothesize it might be untreated fevers or the reasons for fever/pain (such as viral infections) driving the autism link, rather than the acetaminophen washingtonpost.com. Disentangling these effects is notoriously difficult. As epidemiologists point out, in this kind of research “establishing causation…is often impossible” due to the many variables and the inability to do controlled trials on pregnant women washingtonpost.com.
📊 What the Latest Evidence Says
Fast forward to the 2020s, and the evidence remained mixed. Multiple large-scale cohorts – including the well-known Nurses’ Health Study II and the Boston Birth Cohort – have reported statistical links between prenatal acetaminophen use and later diagnoses of autism or ADHD fda.gov. In general, these studies suggest that frequent or long-term use of Tylenol during pregnancy might be associated with a modest increase in risk. Some even indicate the risk is highest when acetaminophen is used chronically throughout pregnancy fda.gov. On the other hand, contrary studies exist that find no significant connection fda.gov. Overall, the scientific literature is divided, and importantly, no study has proven a causal relationship fda.gov.
Recognizing the accumulating (if inconclusive) evidence, researchers called for more scrutiny. In 2023, a group of scientists led by Dr. Andrea Baccarelli (an epidemiologist who is now dean of Harvard’s School of Public Health) performed a comprehensive review and analysis of existing studies. They concluded there is an association worth paying attention to – essentially reinforcing that the signal seen in multiple studies is unlikely to be mere coincidence washingtonpost.comwashingtonpost.com. However, this analysis was steeped in controversy: Dr. Baccarelli had previously served as an expert witness in lawsuits against Tylenol’s manufacturer, and a federal judge had tossed out his testimony in late 2023, calling parts of his analysis “troubling” and criticizing him for cherry-picking studies that found links while ignoring those that didn’t washingtonpost.com. The judge also noted the failure to account for confounders like maternal health conditions or fevers washingtonpost.com. In other words, the court found the evidence for causation too weak, and by December 2023 it dismissed hundreds of lawsuits that had claimed Tylenol caused autism washingtonpost.com.
That might have been the end of the story – science does not support causation, declared the maker of Tylenol in response to the legal win washingtonpost.com. But the story took an unexpected turn in 2025. In a highly unusual move, the issue leapt from the courtroom to the White House. Then-President Donald Trump – who returned to office in the 2024 election – seized on the Tylenol-autism question and made it a public cause célèbre. In September 2025, President Trump forcefully and repeatedly warned pregnant women not to take Tylenol, referencing the very studies that had failed in court washingtonpost.com. During one White House briefing, he linked Tylenol use in pregnancy to autism risk “no less than a dozen times,” amplifying the most alarming interpretation of the unsettled evidence washingtonpost.com. Joining him was his controversial Health and Human Services Secretary, Robert F. Kennedy Jr., a figure known for questioning vaccine safety and other health mainstream views scientificamerican.com. The administration even suggested there might be a treatment to “counter” Tylenol’s supposed effects (promoting an unproven therapy called leucovorin for autism).
This extraordinary government stance stunned medical professionals. The official FDA statement that accompanied the President’s comments was far more measured – acknowledging a “considerable body of evidence” of a possible risk, but also emphasizing that a causal link is unproven and that acetaminophen remains the only safe fever reducer for pregnant women fda.gov. Still, the FDA moved to change Tylenol’s label to note the association with neurological outcomes fda.gov. In effect, the U.S. government was now taking a “precautionary principle” approach: alerting the public to a potential risk despite the scientific uncertainty. “Even with this body of evidence, the choice still belongs with parents,” FDA Commissioner Marty Makary said, adding that many may choose to avoid acetaminophen in pregnancy as a precaution fda.gov. He also acknowledged it “remains reasonable” to use Tylenol in certain scenarios – which likely refers to cases where a high fever or severe pain could pose its own risks fda.gov.
Reaction from the medical and scientific community was swift and largely critical. Many experts expressed outrage, saying the administration had overstepped and was fueling fear based on ambiguous evidence washingtonpost.com. Autism advocacy groups worried this would shame mothers and put them in a cruel bind – afraid to take any medication in pregnancy even when medically necessary. Physicians scrambled to reassure patients: “Independent, sound science clearly shows that taking acetaminophen does not cause autism,” asserted a statement from Kenvue (Tylenol’s manufacturer) in an effort to counter the alarm washingtonpost.com. Doctors stressed that high fevers in pregnancy can be dangerous to a fetus, and Tylenol is often the only recommended fever reducer in those situations fda.gov. Indeed, alternatives like ibuprofen or aspirin are known to cause pregnancy complications (e.g. ibuprofen can harm fetal blood vessels and the kidney in late pregnancy), which is why Tylenol has long been the go-to pain/fever remedy for expectant mothers fda.gov.
Nonetheless, the government’s backing of the autism link lent the idea a new level of credibility in the public eye. Plaintiffs’ lawyers fighting to revive the lawsuits called the administration’s support “helpful…from an atmospheric perspective,” noting that hearing a U.S. President and HHS Secretary validate their claims could influence juries and judges washingtonpost.com. At the same time, researchers like Dr. Baccarelli’s team suddenly found their once-obscure journal article under intense scrutiny and politicization. “It became very politicized with the administration picking it up, and it’s becoming a nightmare in my mind,” said one co-author, who lamented that a nuanced scientific question was now a polarizing public issue washingtonpost.com.
💡 What Should Parents (and Pregnant Women) Do?
Amid the noise, health authorities still emphasize a balanced message. The consensus of most medical organizations can be summarized as follows: If you are pregnant, use acetaminophen only when truly needed, in the smallest effective dose for the shortest time washingtonpost.com. This is actually the same prudent advice that applied even before the autism controversy. No medication is 100% risk-free, and pregnancy is a time to be especially cautious. Non-pharmaceutical measures (rest, hydration, cool compresses for fever, etc.) can be tried first for mild symptoms. But if you have a high fever or significant pain, Tylenol remains the recommended first-line treatment in pregnancy because its known benefits and safety record, when used properly, outweigh the theoretical risks fda.gov. Obstetricians have not advised an outright ban on Tylenol use – doing so could lead to pregnant women either suffering needlessly or resorting to more dangerous alternatives.
In short, the autism link is still unproven. Research continues, and it’s possible that future studies will clarify the connection (for example, there may be specific scenarios or genetic susceptibilities that make acetaminophen riskier for some pregnancies). For now, the mainstream view is that occasional, judicious use of Tylenol during pregnancy is acceptable. Pregnant individuals should always consult their healthcare provider about any medication use. And importantly, they should not be shamed for taking needed medicine – a point many doctors have made in light of the recent scare.
🤔 Myths and Facts about Tylenol
To recap our exploration of Tylenol’s science and controversies, let’s tackle a few myths head-on and set the record straight:
- Myth: “Over-the-counter” means risk-free. Fact: Just because a drug is sold OTC doesn’t guarantee complete safety. Tylenol is very safe at proper doses, but an overdose can be fatal – acetaminophen is actually the leading cause of acute liver failure in the U.S. mayoclinic.org. Always follow dosing guidelines and be mindful of hidden acetaminophen in other products goodrx.com.
- Myth: Tylenol causes autism.Fact: Decades of studies have found a possible statistical link between heavy Tylenol use in pregnancy and a higher chance of autism or ADHD in children fda.gov. However, no causal relationship has been proven fda.gov. Other factors (like the illnesses being treated during pregnancy) may explain the association washingtonpost.com. Health experts still consider Tylenol safe to use when needed during pregnancy, in moderation fda.gov.
- Myth: Tylenol works the same way as other pain relievers. Fact: Tylenol is not an anti-inflammatory medication. Unlike NSAIDs such as ibuprofen or aspirin, it doesn’t reduce swelling or inflammation goodrx.com. Instead, it primarily affects pain and fever signals in the central nervous system, through mechanisms that likely involve prostaglandins and other pathways goodrx.com scientificamerican.com. This difference is why Tylenol is easier on the stomach and doesn’t thin the blood, but also why it won’t help, say, a swollen ankle as much as an NSAID might.
- Myth: No one knows how Tylenol works, so it must be suspicious. Fact: It’s true that scientists are still piecing together acetaminophen’s exact mechanism, but that isn’t due to nefarious mystery – rather, the drug was effective and safe enough that pinpointing its action wasn’t urgent for decades scientificamerican.com. Modern research is finally unraveling those details (even discovering new mechanisms in 2025 sciencedaily.com), which may lead to even safer pain relief options. Tylenol’s therapeutic benefits, however, have been demonstrated in countless trials and real-world use since the 1950s.
- Myth: It’s fine to take Tylenol after drinking. Fact: Combining acetaminophen with alcohol can increase the risk of liver damage, especially with regular or heavy drinking mayoclinic.org. If you’ve consumed alcohol, it’s best to wait several hours before taking Tylenol — or consult a healthcare provider for safer alternatives.
- Myth: Extra Strength Tylenol means it works faster. Fact: “Extra Strength” refers to the amount of acetaminophen per tablet (usually 500 mg vs. 325 mg), not speed. It may provide longer-lasting relief, but it doesn’t kick in quicker. Always check the label and avoid doubling up — more isn’t always better goodrx.com.
🧾 Conclusion
Tylenol holds a unique place in medicine: a humble painkiller so common and trusted that it’s practically synonymous with relief. It’s the pill we reach for without a second thought – to ease a feverish child, to dull a throbbing headache, or to take the edge off an old back injury. That familiarity makes the recent headlines all the more jarring. A TikTok “challenge” turning a safe drug into a daredevil poison. Heated debates over whether that same little pill, taken during pregnancy, might alter a child’s development. It’s a lot to take in, and it’s no wonder people are confused or anxious.
So, what have we learned? First, Tylenol is not a toy and not a candy – abusing it can wreck your liver and end your life. This is a message that parents must convey to their kids in the era of viral challenges. Second, Tylenol is not a silent killer or secret cause of autism – at least not according to the best science we have right now, despite repeated claims of a Tylenol autism pregnancy risk. Pregnant moms should not panic. Use it sparingly and wisely, as always, and consult doctors for guidance. Third, Tylenol’s story is still evolving. We’re discovering new facets of how it works, and we’re vigilantly researching any potential risks. In a way, the saga surrounding this decades-old drug is a case study in how science moves forward: hypotheses are tested, evidence builds (or falls apart), and health recommendations adapt accordingly.
In the end, Tylenol remains – when used with respect and caution – what it has long been billed as: a reliable ally against pain and fever. Its recent entanglements with internet stunts and autism fears serve as a reminder that even the most familiar medicines deserve our respect and understanding. The next time you open your medicine cabinet and see that bottle of Tylenol, you’ll know not just how it might help you, but also the importance of using it responsibly. And if you’re ever unsure, don’t hesitate to ask a healthcare professional – science and good sense go hand in hand when it comes to our health. Stay informed, stay safe, and bust those myths with facts.
Disclaimer:
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have about medications, pregnancy, or your health. Never disregard professional advice or delay seeking it because of something you read here.
Sources:
- Mayo Clinic – Acute Liver Failure: Causes mayoclinic.org
- Indiana University News – New discovery about how acetaminophen works news.iu.edu news.iu.edu
- GoodRx Health – How Does Acetaminophen Work? goodrx.com goodrx.com goodrx.com goodrx.com
- Scientific American – Nobody Knows How Tylenol Really Works scientificamerican.com scientificamerican.com scientificamerican.com
- ScienceDaily – Tylenol stops pain at the nerves (Hebrew University study) sciencedaily.com sciencedaily.com
- SwissInfo – TikTok ‘Paracetamol Challenge’ worries doctors swissinfo.ch swissinfo.ch
- The Independent (UK) – Police warn as children overdose on paracetamol in TikTok challenge independent.co.uk
- Emily’s Hope Charity – Dangerous TikTok paracetamol challenge emilyshope.charity emilyshope.charity
- FDA Press Release (Sept 22, 2025) – Possible Association Between Autism and Acetaminophen fda.gov fda.gov fda.gov
- Washington Post (Sept 25, 2025) – Research tying Tylenol to autism lost in court, then won Trump’s ear washingtonpost.com washingtonpost.com washingtonpost.com washingtonpost.com
- Washington Post – Tylenol maker faces new risk as Trump, RFK Jr. tie it to autismwashingtonpost.com washingtonpost.com washingtonpost.com washingtonpost.com
- WKYT News – Doctor warns parents after boy dies in Benadryl challenge wkyt.comwkyt.com